Published: Nov 2016 | Poster session, “INDOOR AIR 2016” Conference in Ghent, Belgium
Is low indoor humidity a driver for healthcare-associated infections?
Taylor S, Hugentobler W.
Background
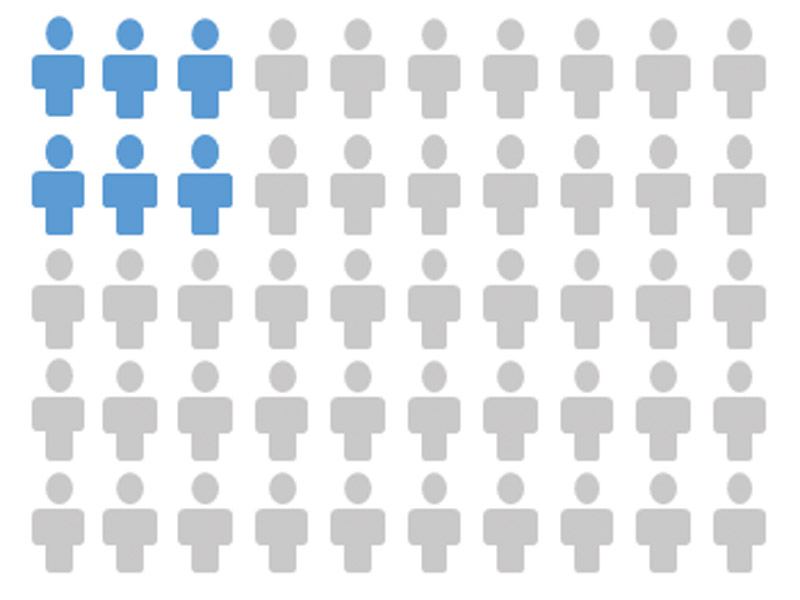
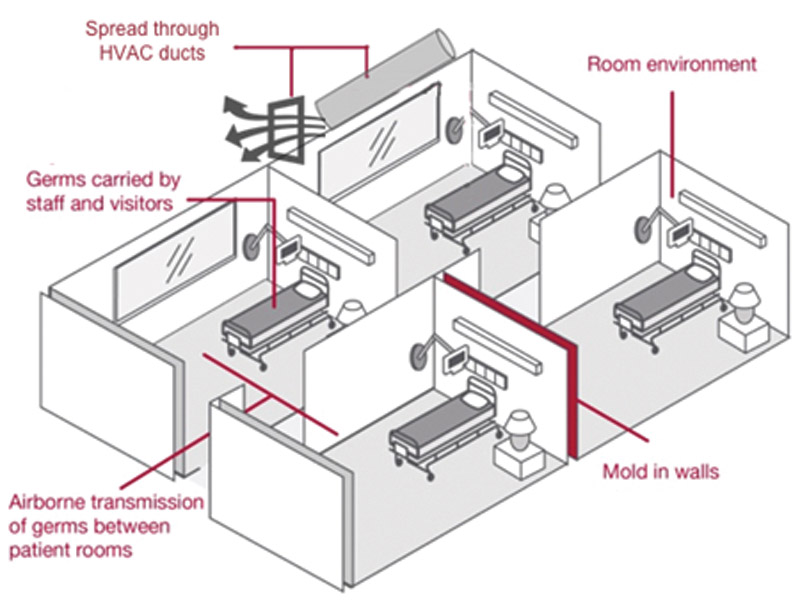
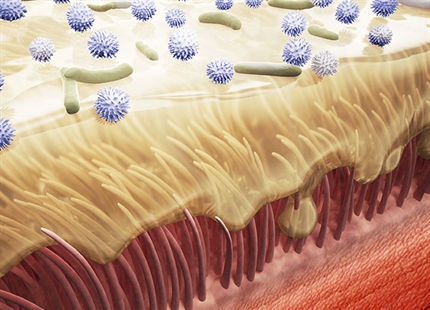
In the US and Europe, errors during in-patient medical care is the 6th leading cause of death (1). A significant portion of this terrible statistic are deaths due to new infections, called nosocomial or healthcare-associated infections (HAIs), that patients acquire while in the hospital. At least 10% of all patients who enter an inpatient healthcare facility for treatment will develop a HAI (2). Tragically, in the US alone, the number of deaths from these infections is over 100,000 annually. What are the environmental factors behind this situation and what more can we do to control the epidemic?
The study
Ten single patient rooms on two floors were monitored for 12 months. Five rooms on one floor were for patients with acute medical or surgical conditions and five rooms on the other floor were for oncology patients
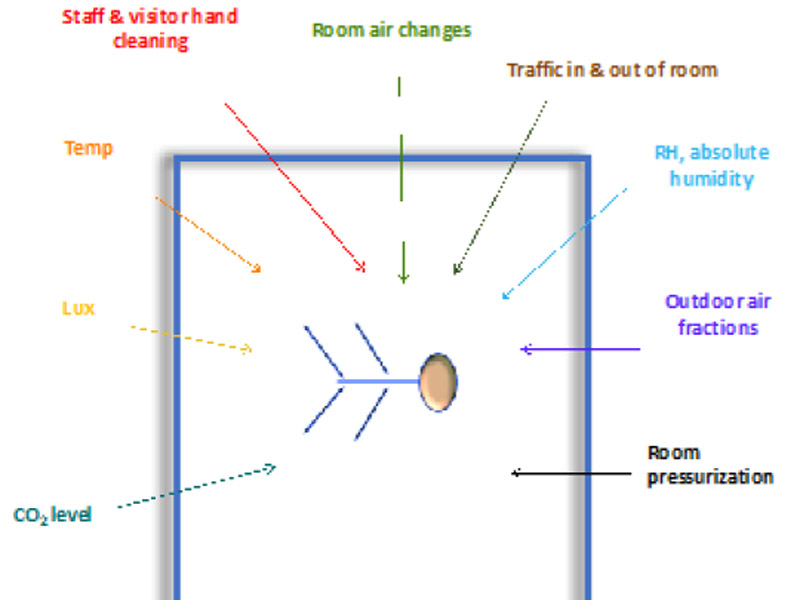
Environmental parameters were measured every five minutes in the ten patient rooms, yielding several million data points over the year-long project.
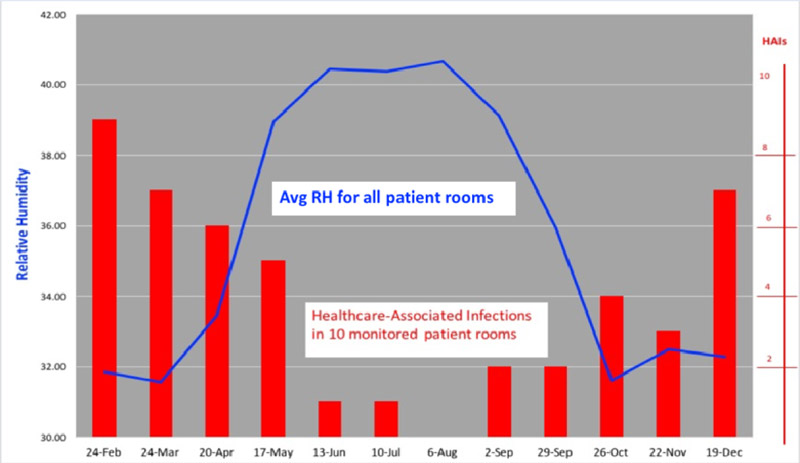
Patient outcomes determined from de-identified records were related to room conditions. Multivariate statistical analysis with linear regression was run to evaluate correlation between indoor measurements and new patient infections (HAIs). HAIs as shown below were found.

Results (part of "The Hospital Microbiome" study)
Low indoor air relative humidity was associated with more patient HAIs. Patient HAIs were inversely associated with relative humidity (RH) as an independent variable in the respective patient care rooms.
Conclusion
Humidification offers an effective yet underutilized preventive measure against healthcare associated infections caused by both bacterial and viral infections. RH from 40 - 60% may provide a safer indoor environment for patients.
References:
1. James J.T. 2013. A New, Evidence-based Estimate of Patient Harm Associated with Hospital Care. J Patient Safety 9(3), 122-128.
2. Classen D.C, Roger R, Griffin F, Federico F, Frankel T, Kimmel N, Whittington J.C, Frankel A, Seger A, James, B. 2011. ‘Global Trigger Tool’ Shows That Adverse Events In Hospitals May Be Ten Times Greater Than Previously Measured. Health Affairs, 30(4), 581–589.